Introduction
One of the overarching goals of modern cancer drug development is to provide more targeted therapies. Unlike conventional treatments, such as chemotherapy and radiation, immunotherapy aims to take advantage of the immune system’s ability to recognize and kill tumor cells while sparing healthy tissues.
Cytokine therapy is a promising form of immunotherapy that works by directly enhancing the immune system’s ability to detect and kill tumors. However, cytokine therapy is complex and there are quite a few roadblocks that are preventing their clinical use. In this article, we’re answering your questions about cytokine therapy to help you get up to speed with the latest advances in this challenging field.
We’ll start off with an introduction to what cytokines are and discuss some of their functional roles before we delve into the use of cytokines in cancer immunotherapy. We’ll discuss FDA approved cytokine therapy drugs, the headwinds the cytokine therapy field is facing, and strategies to address these issues. We’ll also look at how we’re creating novel cytokine therapies here at oNKo-innate, and how next-generation cytokines could revolutionize cancer treatment.
The Basics of Cytokines: Types and Function
Cytokines play a critical role in the function of both the adaptive and innate immune system. Before we discuss the role of cytokines in cancer immunotherapy, let’s investigate the basics: what are cytokines and what do they do?
What are cytokines?
Cytokines are a diverse group of soluble and membrane-bound proteins generated by cells that allow them to communicate – particularly the cells of the immune system. By acting as signaling molecules, cytokines orchestrate immune responses and control inflammation, telling immune cells when and where they need to act.
Cytokines are generally small as far as proteins go, ranging in size from 5 to 70 kilodaltons (kDa). For example, the FDA-approved cytokine therapy interleukin-2 (IL-2) is a mid-range cytokine at around 15 kDa, while IL-12 is a whopping 70kDa.
So, what releases cytokines? Almost every cell in the body can produce cytokines to orchestrate immune responses. Many cytokines are secreted proteins, acting as messengers for communication between cells (paracrine signalling) or altering a cell’s own function (autocrine signalling).
Types of cytokines
As we already mentioned, cytokines are a diverse group of proteins, so there are many different types of cytokines. They are often categorized by their functional categories, including interleukins, chemokines, interferons, colony-stimulating factors (CSF), and tumor necrosis factor (TNF).
What do cytokines do?
The short answer is that cytokines allow cells to communicate. They act as immunomodulators, controlling both the innate and adaptive immune systems’ response to pathogens, injury, or tumorigenesis.
The long answer is… it’s complicated. The functions of cytokines vary considerably because there are so many different types; while some cytokines stimulate immune responses to invading pathogens, other cytokines are critical for putting the brakes on the immune system once the pathogen has been cleared.
Each cytokine can also be highly pleiotropic, meaning that they can have myriad effects. To complicate things further, cytokines don’t just act on the immune system – they are involved in almost all biological processes, from the development of embryos to the aging process.
Once released from a cell, cytokines work by binding to specific cytokine receptors that are expressed on the surface of their target cells. The binding of a cytokine to its receptor then triggers changes in the target cell’s phenotype. This might include the activation, differentiation, proliferation, or suppression of target cells. This means cytokines have the power to control immune cells, either causing or reducing inflammatory responses.
Some cytokines and their effects are well characterized, but in many cases, their function hasn’t been clearly defined – we don’t know what they act on, or their mode of action. Let’s take a look at some examples of the known functions of key cytokines.
Proinflammatory cytokines: Interleukin-12
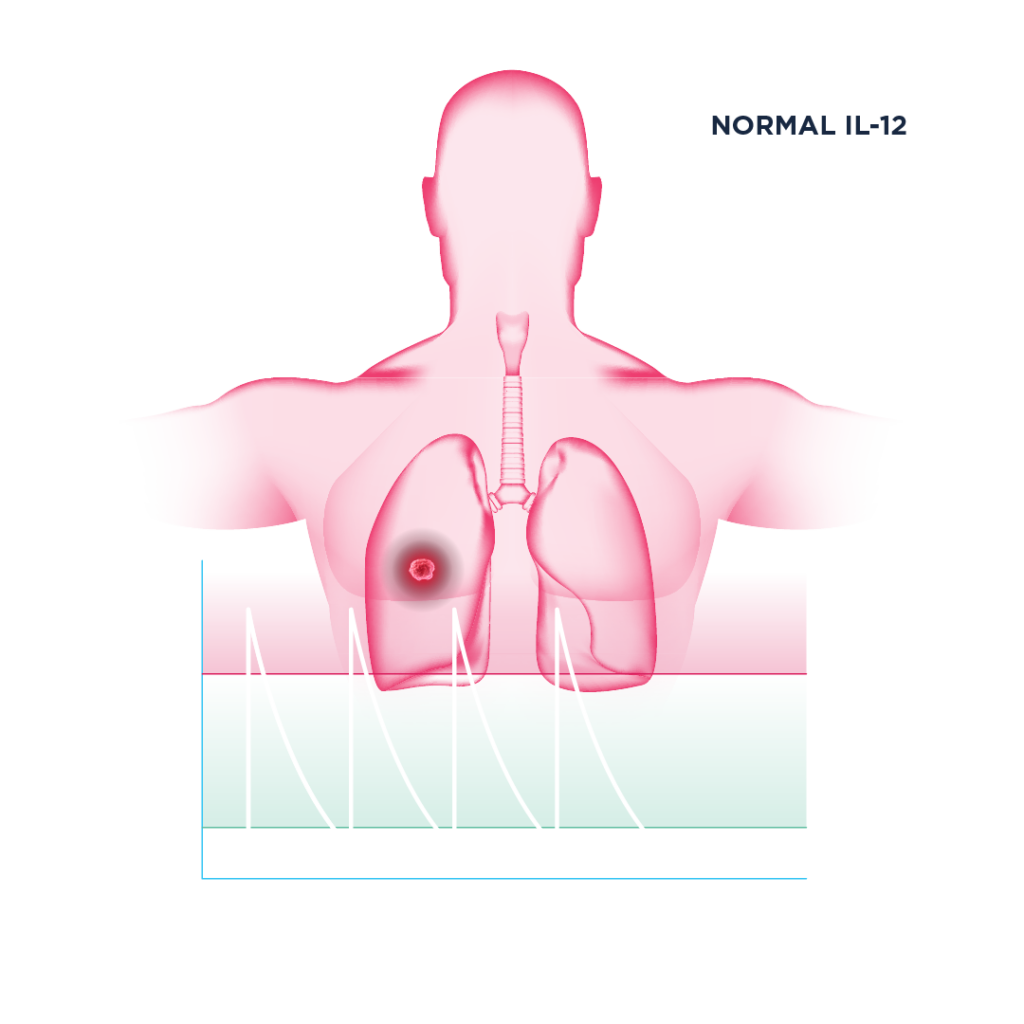
Interleukin-12 (IL-12) is a potent proinflammatory cytokine that has a range of effects on the immune system. Structurally, it is a heterodimeric protein, composed of p35 and p40 subunits. In the context of cancer, IL-12 is primarily produced by macrophages and dendritic cells and exhibits a range of effects within the tumor microenvironment (TME).
IL-12 activates effector immune cells: cytotoxic lymphocytes, like CD8+ T and NK cells. Think of these cells as the front-line soldiers of the immune system, and the tumor as the battlefield. IL-12 causes more soldiers to be recruited into the front line, gives them expert training by causing them to differentiate, and provides them with more powerful weapons in terms of interferon gamma (IFNγ) production.
High levels of IL-12 and IFNγ in the TME inhibits and reprograms suppressive immune cells, like tumor-associated macrophages and regulatory T cells. IL-12 also increases the expression of major histocompatibility complex (MHC)I/II on tumor cells. MHC molecules are important signals that make tumors more “visible” to CD8+ T cells so that they can be killed.
The activation and proliferation of CD8+ T cells and NK cells by IL-12 effectively creates a positive feedback loop in the immune system: secretion of IFNγ activates more macrophages, which in turn secrete additional IL-12 and chemokines, attracting more CD8+ T cells and NK cells to the tumor site. This makes IL-12 incredibly important in terms of optimizing immune recognition and response to cancer.
Anti-inflammatory cytokines: TGF-β
Transforming growth factor-beta (TGFβ) is an anti-inflammatory cytokine that is involved in a wide range of biological processes. It acts as a tumor suppressor, helping clear cancerous cells early on in tumorigenesis. Mutations in the genes that code for TGFβ can cause cancer, as well as other diseases.
However, like many cytokines, TGF-β can be a double-edged sword, and immunologists consider TGF-β to be a bit of a traitor to the immune system due to its ability to suppress NK and CD8+ T cell function. In the later stages of cancer, it can actually promote cancer growth and metastasis – essentially acting as a proto-oncogene. Many different types of tumors are associated with dysregulated TGFβ signaling, including lung, breast, prostate, and colon cancers.
Cytokine vs. chemokine: What’s the difference?
Chemokines are a specialist type of cytokine that control the trafficking of immune cells throughout the body. Their name comes from the fact that they are chemotactic cytokines, directing the movement of circulating leukocytes (white blood cells) throughout the body and recruiting them to sites of inflammation or injury. In the context of cancer, chemokines are essential for helping immune cells find and infiltrate tumors.
Cytokine Therapy for Cancer Treatment
Administration of cytokines to cancer patients has been an area of extensive research over the past 40 years due to their ability to modulate the immune response to cancer – an approach termed cytokine therapy. Let’s explore how cytokine therapy works, a few examples of cytokine therapies, some of the ongoing challenges in the cytokine therapy field, and a few of the approaches to overcoming these obstacles.
What is cytokine therapy?
Cytokine therapy usually involves delivering recombinant cytokines systemically to treat disease. Cytokine therapy is most common in cancer and disorders of the immune system, including autoimmune disease.
The use of cytokines in cancer immunotherapy aims to activate the immune system, particularly those soldiers we mentioned earlier whose job it is to kill cancer cells: CD8+ T cells and NK cells. Cytokine therapy exploits the ability of cytotoxic lymphocytes to distinguish between healthy tissues and tumor cells, preferentially killing the latter.
Cytokine therapy works differently from conventional immunotherapies, such as immune checkpoint blockade (ICB); while ICB prevents cytotoxic lymphocytes from being ‘switched off’ when responding to tumors, cytokine therapy helps these cells “switch on” when they encounter tumors.
Because cytokines are able to activate immune cells, cytokine therapy is being explored as a method to heat up immunologically cold tumors that have failed to respond to ICB. Read more about cold tumors in our article below.
Are there any FDA approved cytokine therapy drugs for cancer?
Currently, there are only two FDA approved cytokine therapy drugs that are used in cancer immunotherapy. One of these is proleukin, also known as aldesleukin. This drug is a recombinant form of IL-2 and was approved by the FDA for the treatment of both metastatic melanoma and metastatic renal cell carcinoma. The other is interferon alpha (IFN-α), which was approved for the treatment of blood cancers and melanoma.
Obstacles to the successful clinical translation of cytokine therapies
Despite the power of many pro-inflammatory cytokines in mounting immune responses to tumors, there are several key issues that have prevented the clinical translation of cytokines in cancer immunotherapy, including toxicity, limited half-life, lack of tumor-targeting, and the induction of immunosuppression via regulatory T cells or myeloid cells. These obstacles currently prevent cytokine therapy from being regularly prescribed as a cancer treatment.
The most problematic issue is that systemic administration of cytokines causes major side effects or toxicities, which can be fatal. This issue is exacerbated by the fact that cytokines have an extremely short half-life in vivo; frequent administrations of high doses are typically required for cytokine therapy to be effective.
As we mentioned earlier, cytokines are highly pleiotropic, affecting many different types of cells. This means that even if the intended outcome of cytokine therapy is achieved, there can also be other unintended, and sometimes negative, consequences.
One such example is IL-10 (pegilodecakin), a cytokine therapy which has been trialed in cancer patients due to its ability to increase the number and function of tumor-specific T cells. The problem is that IL-10 is also an important anti-inflammatory cytokine – it’s involved in regulatory T cell development, so it can actually suppress monocyte and macrophage activity, which is not desirable in cancer patients.
Current approaches to next-generation cytokine therapy
The holy grail of cytokine therapy is to design molecules that have drug-like characteristics, retaining their on-target anti-tumor activity while minimizing toxicity. Many research organizations are dedicating large resources to this endeavor, attempting to circumvent the issues that have historically plagued the cytokine therapy field.
Unfortunately, several recent high-profile next-generation cytokine therapy drugs that have attempted to achieve this holy grail have failed early in clinical trials. These setbacks highlight the need for a deeper understanding of the on-target mechanisms driving clinical efficacy versus toxicity. Explore the main approaches to next-generation cytokine therapy in Table 1 below.
Table 1: Current Approaches to Next-Generation Cytokine Therapy
| Engineered cytokine variants | Modifications amplify the therapeutic properties of the cytokines, such as altering their binding affinity for their receptor, extending their half-life by fusing them to the Fc region of an antibody, or biasing their activity within the TME by including a masking domain that is cleaved by tumor enzymes. |
| Multi-specific cytokines | The cytokines can be fused with antibodies or targeting ligands to improve their delivery to the TME. |
| Selective receptor agonists | A subset of cytokine receptors is activated to achieve a differentiated response, rather than broad activation of the cytokine receptor complex. |
| Cytokine checkpoint inhibitors | Small molecule drugs enhance cytokine receptor signalling and duration in immune cells, so they can respond to endogenous cytokines present in tumors. |
| Cytokine antibodies | Antibodies augment the binding affinity of endogenous cytokines to a particular receptor or cell type, redirecting them to the intended target. |
| Small molecule agonists | Small, synthetic molecules mimic the effects of cytokines, selectively activating cytokine receptors. |
| Nanoparticle delivery | Cytokines can be packaged in or attached to the surface of nanoparticles, allowing controlled release and targeted delivery of cytokine therapy. |

The Future of Cytokine Therapy: Engineered Variants and Cytokine Checkpoint Inhibitors
At oNKo-innate, we’re rethinking immuno-oncology and developing bold new strategies to drive safe and effective cytokine therapies into the clinic. As a leading Australian immuno-oncology company, we’re actively reshaping the future of cytokine therapy, with two main cytokine therapy products in our pipeline: oNKo-001 and oNKo-037.
oNKo-001: An engineered, reduced-potency IL-12 cytokine
The oNKo-001 cytokine therapy is our take on engineered cytokine variants and aims to harness the potent anti-tumor efficacy of IL-12 to treat a variety of solid tumors, particularly hard-to-treat cancer types that historically have not responded to conventional immunotherapies.
We’ve created a modified IL-12 fusion protein with significantly reduced affinity to its receptor, the IL-12RB2 receptor. This reduction in potency means that oNKo-001 avoids the systemic activation of peripheral IL-12R-expressing immune cells, which contribute to IL-12’s dose-limiting toxicity. We fused this reduced-potency IL-12 to the fragment crystallizable (Fc) region of an antibody, which maximizes its half-life in vivo and reduces the need for repeat doses, all while retaining its anti-tumor activity.
The reduced affinity of oNKo-001 to the IL-12RB2 receptor adds to its extended half-life and pharmacokinetic properties. It minimizes how quickly the drug will bind to, and be used up by, non-target cells so that it has maximal exposure to tumor-infiltrating lymphocytes instead.
oNKo-037: An IL-15 cytokine checkpoint inhibitor
oNKo-037 takes a very different approach to traditional cytokine therapy and is classed as a cytokine checkpoint inhibitor, based on interleukin-15 (IL-15). IL-15 is a key cytokine in supporting the fitness and function of CD8+ T cells and NK cells in the TME. Our previous work suggests IL-15 concentrations in tumors are limiting; anti-tumor immunity is improved when IL-15 levels are increased, yet endogenous IL-15 levels are often low.
We conducted functional genomic screens in primary human immune cells to determine which targets affected sensitivity to IL-15 and found a small number of druggable targets, including oNKo-037. When inhibited, it increases the sensitivity of CD8+ T cells and NK cells to low levels of endogenous IL-15. This means we can increase anti-tumor activity exactly where it’s needed, while avoiding the toxicity associated with systemic administration of cytokines like IL-15.
Moving Next-Generation Cytokine Therapies into the Clinic
One of the most interesting questions as we move forward in the cytokine therapy field is how broadly cytokine therapies can be employed, since conventional immunotherapies such as ICB are restricted to specific tumor types. It will be fascinating to assess whether cytokine therapy can be used to treat refractory cancers that have not responded to other treatments like ICB, as well as other tumor types that cannot be treated with ICB in the first place.
With more development and research, cytokines may emerge as stand-alone therapies, employed as combination therapies with ICB, or could even be used to enhance cellular immunotherapies and broaden the range of cancers they can treat. At oNKo-innate, we hope to bring both of these innovative cytokine therapy candidates to the clinic in the near future so that we can start transforming the lives of patients.
We hope this article helped you understand the basics of cytokine therapy and why we’re so passionate about it here at oNKo-innate. We believe we’re only just beginning to scratch the surface of the true potential of cytokine therapy. If you want to learn more about immuno-oncology and cytokine therapy, watch this space – we’ll be posting more articles like this soon!
You can also follow us on X and LinkedIn for regular updates.